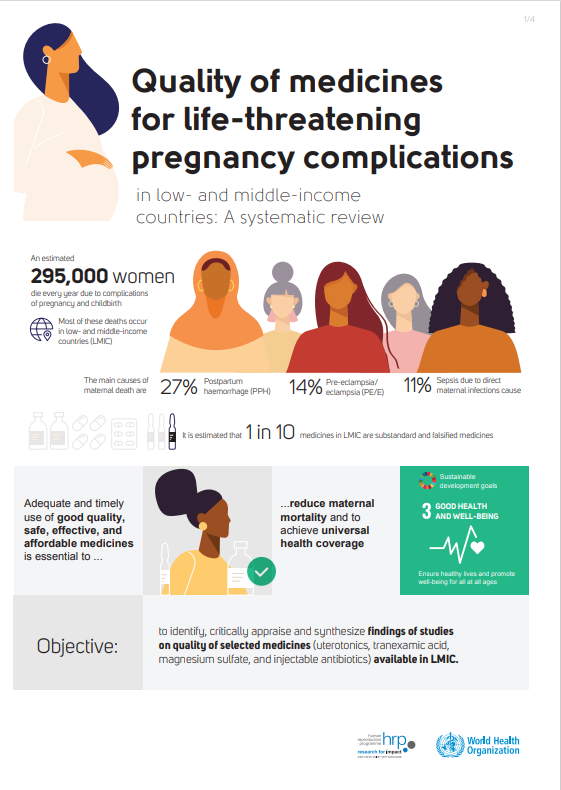
The research ‘Quality of medicines for life-threatening pregnancy complications in low- and middle-income countries: A systematic review’ published in 2020 by Maria Regina Torloni, Mercedes Bonet, Ana Pilar Betrán, Carolina C. Ribeiro-do-Valle, Mariana Widmer addresses concerns about the quality of medicines available in low- and middle-income countries (LMIC) to manage hemorrhage, pre-eclampsia/eclampsia and sepsis. It aims to identify, critically appraise, and synthesize the findings of studies on the quality of these three types of medicines available in LMIC.
An estimated 295,000 women die every year due to complications of pregnancy and childbirth. Most of these deaths occur in low- and middle-income countries (LMIC) and could be avoided with adequate healthcare. Postpartum hemorrhage (PPH), pre-eclampsia/eclampsia (PE/E), and sepsis due to direct maternal infections cause 27%, 14% and 11% of all maternal deaths, respectively and are also major contributors to severe maternal morbidity. The adequate and timely use of good quality, safe, effective, and affordable medicines is essential to achieve universal health coverage and reduce maternal morbidity and mortality.
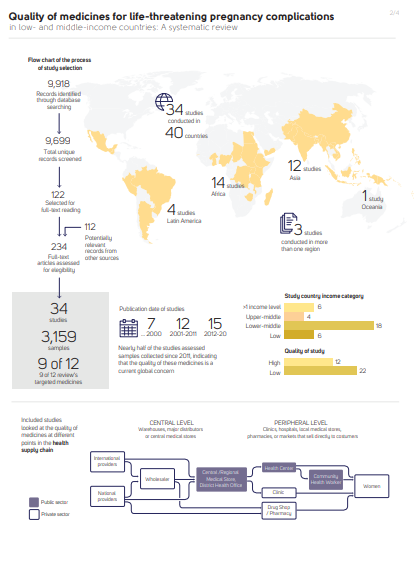
Main findings: identified 9699 unique citations and included 34 studies (3159 samples from 40 countries) in the review. Most studies (65%) had low quality (scores <6/12).
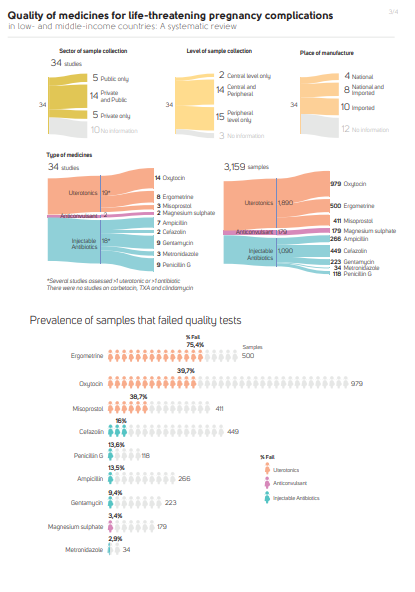
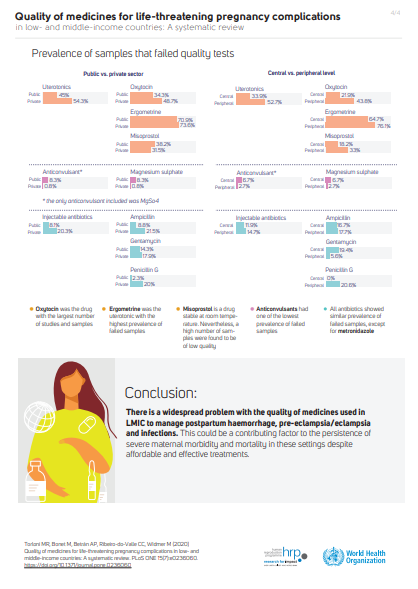
Overall, 48.9% of 1890 uterotonic samples (19 studies) failed quality tests; failures rates were 75% for ergometrine and nearly 40% each for oxytocin and misoprostol. The overall prevalence of failed injectable antibiotics (1090 samples, 18 studies) was 13.4%, ranging from 2.9% for injectable metronidazole (34 samples, 3 studies) to 16.0% for cefazolin (449 samples, 2 studies). The prevalence of low quality magnesium sulphate (179 samples, 2 studies) was 3.4%. They did not find any studies on the quality of carbetocin, tranexamic acid, or clindamycin.
The review concludes that there is a widespread problem with the quality of medicines used to manage life-threatening maternal conditions in LMIC. This can be a contributing factor to high maternal mortality rates in these regions.